Download the whole case study as a PDF file
Anne has been married to Arthur for over 70 years. Arthur has end stage Chronic Pulmonary Disease and is nearing the end of his life.
This case study considers end of life care and the needs of people who are living with dying. It looks at the impact of bereavement and social isolation, and also touches on religion and spirituality.
When you have looked at the materials for the case study and considered these topics, you can use the critical reflection tool and the action planning tool to consider your own practice.
Name: Anne Woolsey
Gender: Female
Age: 92
Ethnicity: White British
Download resource as a PDF file
First language: English
Religion: Christian faith (Anglican Church)
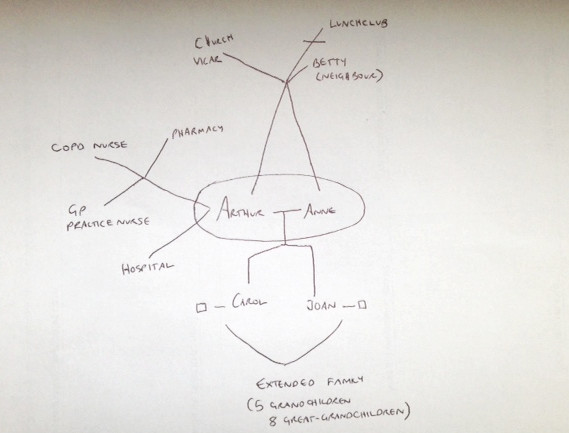
Anne is married to Arthur, 94. They have been married for over 70 years and live in their own bungalow in a village. Anne and Arthur have two daughters, five grandchildren and eight great grandchildren. The family are quite dispersed across the country. Their nearest daughter Carol, who lives 40 miles away, visits twice a month. Daughter Jean visits every other month. Both daughters phone regularly. Their neighbour Betty calls in most days.
Arthur has end stage Chronic Pulmonary Disease (COPD) and is nearing the end of his life. Arthur is currently housebound, using oxygen at home. He has support from a Community COPD nurse. Anne has provided care for Arthur for eight years, and the support that he needs is increasing. The COPD affects Arthur’s mobility and he is unable to get to the toilet in time at night. Most mornings he awakens with soiled sheets which distresses him. Anne continues to look after the home and has started to manage the finances, which previously Arthur did. Anne and Arthur find it difficult to talk with each other about Arthur’s death. They would both like Arthur to die at home, with his wife and daughters.
Anne’s health is generally good, though she has mild arthritis and takes tablets for stable angina. However, she is becoming less strong and more tired. Anne has some hearing impairment and finds it difficult to read small print. Anne devotes her time to caring for Arthur and no longer goes to church. Both were previously active in the community and attended a local lunch club. Anne is determined to be there for Arthur and does not like to leave him, even with someone else. Her main concern is that she will not be able to support Arthur till the end. Anne is beginning to find it difficult to look after the home and garden, and to feel quite isolated. She is not confident in managing the family finances and is not sure how she will manage when Arthur is gone.
Carol is concerned about her mother not sleeping well and looking tired. She rings the local authority. You go out and complete the initial assessment and support plan with Anne. As part of this you talk to Arthur, Carol, Jean and Betty.
Download resource as a PDF file
Personal details
Name: Anne Woolsey
Address: 12, Oak Tree Close, Hawton ZZ2 Z22
Telephone: 01654 654321
Email: N/A
Gender: Female
Date of birth: 28.06.23 Age 92
Ethnicity: White British
First language: English
Religion: Baptised C of E
GP: Dr Philps, Oak Tree Surgery
Chronology completed by
Name:
Role:
Organisation:
Date chronology completed: 15 February 2016
Date shared with person: 15 February 2016
| Date | Life event | Outcome and/ or response |
| 08.08.45 | Anne Mary Marshall married Arthur Eric Woolsey (dob 18.11.21), a local builder | Married name Mrs Anne Mary Woolsey |
| 25.11.53 | Birth of first child | First daughter, Carol Anne Woolsey |
| 12.04.55 | Birth of second child | Second daughter, Jean Lesley Woolsey |
| 31.01.82 | Husband Arthur retired from the building trade. He had carefully planned for his retirement, having always managed the family finances. | Arthur and Anne enjoyed good health in their early retirement, and were active within the local community, particularly with their local church. |
| 17.09.88 | Arthur has been a smoker most of his life and his breathing begins to affect his mobility. Anne and Arthur decide to move to a bungalow. | Anne and Arthur moved home. They bought a bungalow so that Arthur did not have to worry about stairs as his breathing worsened. They continued to enjoy an active retirement following the arrival of five grandchildren during the last decade. |
| 22.03.08 | Arthur attends his local GP surgery with chronic breathing difficulties and is referred to the local hospital for investigation. | Diagnosis of Chronic Obstructive Pulmonary Disease (COPD. It is thought that his work in the building trade may have been a contributory factor, along with his smoking habit. Arthur did give up smoking at some point in the ten years before being diagnosed. |
| 03.07.15 | Arthur admitted to hospital with chronic chest infection and difficulties breathing. | Arthur diagnosed with end stage COPD. Anne now provides all personal care for Arthur. Anne is starting to become more isolated as she does not feel happy leaving Arthur. |
| 17.07.15 | Referral to Community COPD nurse service as part of hospital discharge plan. Arthur now has oxygen at home. | COPD Nurse begins to visit every few weeks to check on Arthur and bring medication. |
| 03.01.16 | Daughter Carol is concerned about her mother not sleeping well and looking tired. Referral to social services. | Social worker phones to arrange an assessment visit. |
| 15.01.16 | Initial SW assessment visit to Arthur and Anne. | SW arranges to visit again when Carol is next visiting her parents to continue the assessment.
Arthur agrees to have his own assessment as part of this visit. |
| 11.02.16 | Second assessment visit with Carol, Jean and Betty (neighbour) present. | Carer’s assessment and support plan completed. |
| 15.02.16 | Paperwork completed. | Sent to Anne. |
Anne Woolsey
Download resource as a PDF file
What others like and admire about me
My marriage to Arthur – we’ve loved each other for seventy years
I’m very fit for my age
I’ve always helped out in the parish and I used to run the Mother’s Union
My big family – we are fortunate to have eight great-grandchildren
What is important to me
Looking after Arthur
Staying on top of the house work
Having a bit of a sit together with Arthur
Someone to help with the finances
My faith and my parish
Looking after myself
How best to support me
Talk to me about what is happening to Arthur
Be honest about what you can do
Let me know who to contact if the worst happens
Don’t expect me to use a computer
Help me with the finances
Let my family know that I need help now
Download resource as a PDF file
Anne’s Ecogram
Name: Anne Woolsey
Date completed: 15 February 2016
Download resource as a PDF file
Carers Assessment
About me
Name: Anne Woolsey
Address: 12, Oak Tree Close, Hawton ZZ2 Z22
Telephone: 01654 654321
Email: N/A
Gender: Female
Date of birth: 28.06.23 Age 92
Ethnicity: White British
First language: English
Religion: Baptised C of E
GP: Dr Philps, Oak Tree Surgery
How would you like us to contact you?
By telephone or letter
Do you need any support with communication?
I need written information to be in large print
About the person/ people I care for
My relationship to this person: Wife
Name: Arthur Woolsey
Address: 12, Oak Tree Close, Hawton ZZ2 Z22
Telephone: 01654 654321
Email: N/A
Gender: Male
Date of birth: 18.11.21 Age 94
Ethnicity: White British
First language: English
Religion: Baptised C of E
GP: Dr Philps, Oak Tree Surgery
Please tell us about any existing support the person you care for already has in place. This could be home care, visits or support from a community, district or community psychiatric nurse, attending any community groups or day centres, attending any training or adult learning courses, or support from friends and neighbours.
Our two daughters help out when they can – Carol is nearest, 40 miles away. She visits a couple of times a month and our other daughter, Jean, tries to come as often but it’s more like every 2 months or so. Jean and Carol each phone every week to see how we are.
Our neighbour, Betty – she pops in nearly every day now to see if we need anything. We’ve been friends for many years and she’s not young herself.
The GP and nurse at the surgery are very good though we don’t like to bother them, they are very busy.
The COPD Nurse stops by every few weeks to check on Arthur and bring his medication.
Vicar – we don’t get to church much now a days but the vicar comes round now and then.
We used to go up to a lunch club at the church but we’ve stopped going lately.
Carol does the heavy shopping and helps with the housework when she comes. Jean and Carol both look things up for their parents and advise them as best they can. Both take Anne and Arthur out for short drives when they visit.
The things I do as a carer to give support
Please use the space below to tell us about the things you do as a carer (including the emotional and practical support you provide such as personal care, preparing meals, supporting the person you care for to stay safe, motivating and re-assuring them, dealing with their medication and / or their finances).
Arthur has Chronic Obstructive Pulmonary Disease (COPD) – Arthur did give up smoking about ten years ago. He was in the building trade all his life which the hospital said may have been a contributory factor, along with his smoking. We’ve been told he probably won’t make it to next Christmas, but that is what we hope for all being well.
This is what I do for Arthur and me:
- Get my husband out of bed and get him washed and dressed.
- The bed clothes are usually soiled so I get the bed stripped and into the wash.
- Make him breakfast and help him eat it.
- Give him his tablets.
- Do the housework – I try to do a few jobs each day, rather than doing one big clean – looking after Arthur takes up so much of my time.
- Deal with the visitors to the house – social worker, COPD nurse, GP – I try to have them come in the morning.
- Pop out to get some shopping- just to the local shops, little and often as I can’t carry a heavy shop any more.
- Do us a bit of dinner, though Arthur doesn’t eat so much these days
- In the afternoon, I might look at trying to pay some bills. I’m trying to find out about power of attorney.
- Make our tea
- Tidy up and get us ready for bed
- Make Arthur a drink and give him his tablets
- Sort out the oxygen
- Lock up for the night.
How my caring role impacts on my life
Please use the space below to tell us about the impact your caring role has on your life.
Arthur and I have been married for over 70 years – he’s my world. He’s always sorted out the finances, paid our bills and made sure we have enough to go round. I’m trying to do the paperwork now but I’m very worried about how I’ll cope, I’ve never had to do this before. I’ve never written a cheque and I’m worried I’ll get it wrong.
I wake up in the morning still tired, it’s usually a disturbed night’s sleep, but I have to get on with it as Arthur needs washing and dressing. He’s often in a mess poor thing.
I make sure we have time to sit together and relax, I try to do things little and often – I’m very lucky to still have my health.
When Arthur nods off I try to do the bills but I end up nodding off too then I get very worried that things will fall behind. I don’t know how I will manage when Arthur is gone.
The girls are very good and the grandchildren ring now and then. I try not to make a fuss, they’re all so busy. The girls know I’m very worried about losing Arthur. I can’t bear to talk about it, I just want to make the most of the time we have left.
This year I’ve not been able to do my planting and keep the bungalow up as I’m used to. I am feeling more tired and I suppose the main fear I have is that I won’t be able to keep caring for Arthur to the end. I know I need to look after myself but I’m sometimes too tired to eat and I’m not sleeping well.
I have lost touch with the church and the people we used to see. Sometimes I feel quite alone.
What supports me as a carer?
Please use the space below to tell us about what helps you in your caring role.
Betty next door is such a good friend, she does her best but she is not young herself.
The doctor is understanding but there’s not much he can do now.
The nurse up at the surgery has known us a long time and I can ring her if I’m worried.
The Community COPD nurse comes once a month and checks how Arthur is.
Carol and Jean help with the shopping and try to help me with the bills and letters but Arthur and I have always managed these things ourselves, I don’t want to let him down.
Carol does the heavy shopping for me once a month.
We see the Vicar now and then. The church has always been a comfort to me.
My feelings and choices about caring
Please use the space below to tell us about how you are feeling and if you would like to change anything about your caring role and your life.
I am determined to look after Arthur until the very end. I need to stay well enough to do that.
Arthur and I both want me to help him with personal care, not a stranger.
I want to be able to manage and do my best for him.
I would like to have more sleep so I don’t nod off when I should be sorting things out.
I wish the girls were closer so that they could come more often.
When the time comes I would like Arthur to die at home with me and his girls. This is what he wants too though he doesn’t like to talk about it.
I need to make sure that I can take care of the bungalow and the garden, and that the bills are sorted out.
Information, advice and support
Let us know what advice or information you feel would help you and what sort of support you think would be beneficial to you in your caring role.
Some help with sorting out the bills and keeping on top of the paperwork like Arthur would want me to.
I would like the garden to look better so Arthur could sit outside sometimes.
Some back up in the mornings with changing the bed and getting the laundry done.
Someone to talk to about how to manage all of this. I don’t like to talk about it in front of Arthur. He finds it very difficult to talk about leaving me and he doesn’t want to talk about what he would like to happen at the end or after he’s gone. I don’t want to think about it. We have always said we would stay together till the very end. That is all I want, to be together in our own home. We never made our wills and I don’t have power of attorney or anything like that.
Conclusion
To be used by social care assessors to consider and record measures which can be taken to assist the carer with their caring role to reduce the significant impact of any needs. This should include networks of support, community services and the persons own strengths. To be eligible the carer must have significant difficulty achieving 1 or more outcomes without support; it is the assessors’ professional judgement that unless this need is met there will be a significant impact on the carer’s wellbeing. Social care funding will only be made available to meet eligible outcomes that cannot be met in any other way, i.e. social care funding is only available to meet unmet eligible needs
Date assessment completed 15 February 2016
Social care assessor conclusion
Anne is providing significant daily support to her husband aged 94 who has COPD and is reaching the end of his life. At 92 years of age herself, Anne’s health is generally good though she is increasingly frail and says she tires more easily these days. The couple live together in the matrimonial home. Her husband has monthly visits from the COPD nurse. Their nearest daughter visits once a month and does the heavy shopping. They have one other daughter who visits when she can, about every other month, and phones regularly. Their neighbour, Betty, a pensioner herself, pops in most days to check they are ok. Anne is very organised and has supported Arthur for many years while looking after the home. However, Anne’s caring role is starting to impact on her health. She says that she is starting to feel increasingly tired and has disturbed nights. Anne does not feel confident in managing the family finances and is beginning to find it difficult to manage the home and garden. Anne would like to continue looking after Arthur at home “until the end”. Both want to be together and for Arthur to die at home with his family. Anne would benefit from support to enable her to manage the demands on her, and to have some more time to relax and just be with Arthur. They each find it hard to talk about Arthur’s death in front of the other. Arthur finds it difficult to say what he would like to happen at the end and to plan for this. Anne has previously found comfort in the church but has become more isolated recently. Anne would benefit from some emotional support for herself and for her family, as well as practical help, advice, and support to manage finances. This will enable her to continue as Arthur’s main carer, which is what both of them want, and to maintain her own health and wellbeing.
Eligibility decision Eligible for support
What’s happening next Create support plan
Parallel assessment for Arthur Woolsey
Completed by
Name
Role
Organisation
Signing this form (for carer)
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Name:
Signature:
Download resource as a PDF file
About me
About me
Name: Anne Woolsey
Address: 12, Oak Tree Close, Hawton ZZ2 Z22
Telephone: 01654 654321
Email: N/A
Gender: Female
Date of birth: 28.06.23 Age 92
Ethnicity: White British
First language: English
Religion: Baptised C of E
GP: Dr Philps, Oak Tree Surgery
About the person/ people I care for
My relationship to this person: Wife
Name: Arthur Woolsey
Address: 12, Oak Tree Close, Hawton ZZ2 Z22
Telephone: 01654 654321
Email: N/A
Gender: Male
Date of birth: 18.11.21 Age 94
Ethnicity: White British
First language: English
Religion: Baptised C of E
GP: Dr Philps, Oak Tree Surgery
Support plan completed by
Name
Role
Organisation
Support plan
Date of support plan: 15 February 2016
This plan will be reviewed on: 15 April 2016
Signing this form
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Name:
Signature:
Anne has asked for her assessment and support plan to be considered as part of Arthur’s assessment. Arthur is happy for his assessment and support plan to be considered as part of Anne’s assessment and support plan.
End of life
Research shows that people who had seen palliative care social workers were extremely positive about their support. Yet the same studies found that there was an unmet demand for palliative care social work; too many people miss out on social work (Moriarty and Manthorpe 2016).
Association of Palliative Care Social Workers in collaboration with the former College of Social Work and Making Waves Lived Experience Network/OPEN FUTURES Research, with support from the British Association of Social Workers and Hospice UK (2016) The role of social work in palliative, end of life and bereavement care http://www.apcsw.org.uk/resources/social-work-role-eol.pdf
Milne A, Sullivan MP, Tanner D, Richards S, Ray M, Lloyd L, Beech C and Phillips J (2014) Social work with older people: a vision for the future
National Palliative and End of Life Care Partnership (2015) Ambitions for Palliative and End of Life Care: A national framework for local action 2015-2020
Marie Curie (2012) Committed to carers: Supporting carers of people at the end of life
Gold Standard Framework (2011) The surprise question
Video
Dawn French introduces ‘Living with dying’ on healthtalk.org
Dying Matters, I’m having a very good death
Tools
Living with dying
Research points to the need to put the individual and their surrounding family or carers at the heart of end of life and palliative care (Alcide and Potocky 2015, Ewing 2015, Hansen 2015, Karla et al 2014, Beresford et al 2006).
- Association of Palliative Care Social Workers in collaboration with the former College of Social Work and Making Waves Lived Experience Network/OPEN FUTURES Research, with support from the British Association of Social Workers and Hospice UK (2016) The role of social work in palliative, end of life and bereavement care
- SCIE (2013) Dying well at home: the case for integrated working
- NICE guidance on Care of dying adults in the last days of life
- NHS Choices: Planning ahead for the end of life
Video
- SCIE, Dying at home
Bereavement support
An important factor in the research across social work with carers was an understanding of life change and course, and transition with particular reference to loss and bereavement.
- Association of Palliative Care Social Workers in collaboration with the former College of Social Work and Making Waves Lived Experience Network/OPEN FUTURES Research, with support from the British Association of Social Workers and Hospice UK (2016) The role of social work in palliative, end of life and bereavement care
- Dying Matters: raising awareness of death, dying and bereavement
- The National Council for Palliative Care. Who cares? Support for carers of people approaching the end of life
- NHS Choices: When someone you care for dies
Video
Tool
Loneliness and isolation
Evidence about the asset based approach to social work has a generic relevance to work in the community with carers (Klee 2014).The carers strategy demonstrator sites identified the benefits of workers from voluntary organisations assisting social workers undertake carer’s assessments (Yeandle 2011).
- SCIE Resource Guide: Preventing loneliness and social isolation among older people
- RiPfA Key Issue: Building community capacity
- Carers UK (2015) Alone and caring: Isolation, loneliness and the impact of caring on relationships
- Age UK and The campaign to end loneliness (2015) Promising approaches to reducing loneliness in later life
- Age UK (2015) Loneliness and Isolation Evidence Review
- Age UK (2015) Loneliness in Later Life Evidence Review
- Age UK (2013) Supporting Older Carers of Those Nearing the End of Life, Lancaster University Evaluation of Six Pilot Projects. Final Report
- Public Health England (2015) Reducing social isolation across the lifecourse
- Carers UK as part of the Jo Cox Loneliness Commission (2017) The world shrinks: Carer loneliness
- CarersUK (2017) Make connections, get support
Video
- SCIE, Promoting wellbeing
Tools
- Tool 4: Supporting older carers, spheres of support
- Tool 5: Reducing loneliness
Religion and spirituality
Common factors identified in the research for social work practitioners working with adults and their carers included information, advice and guidance – having the specialist knowledge or knowing where to signpost people – assessment and the processes of carer-directed self-support, and using knowledge and skills to work with the whole network of relevant people.
- The Institute for Research and Innovation in Social Services (2013) Spirituality and ageing: implications for the care and support of older people
- Health Talk: religion, faith and philosophy
- Furness S and Gilligan P (2010) Social Work, Religion and Belief: Developing a Framework for Practice, British Journal of Social Work, 40 (7), pp 2185-2202
- Tool 6: Principles for reflection on religion and belief
Download the tool as a PDF
Tool 1: What social workers offer at end of life
These are some of the particular ways that all social workers support end of life and bereavement care.
You can use this tool to consider the role of social workers in end of life care and how your role can support people who are dying or bereaved.
1. Discussions as the end of life approaches
Social workers:
- Build relationships that enable discussions to take place
- Sensitively initiate discussions about the future
- Ensure everyone is involved who needs to be
- Refer people to other professionals for more support when appropriate.
2. Assessment, care planning and review
Social workers:
- Focus on promoting wellbeing and achieving what matters to each person
- Look at all needs and strengths
- Consider preventative services and changing needs in the future
- Advocate for support from other services
- Ensure people get benefits they are entitled to
- Balance individuals’ and unpaid carers’ needs
- Advise on and implement the relevant legislation and policy to support decision making
- Sensitively apply social care law, policy and practice to safeguard people when needed.
3. Co-ordination of care and delivery of high quality care in different settings
Social workers:
- Ensure people are at the centre of their care and have information about who is doing what
- Build relationships with specialist palliative care providers
- Support communication and information sharing so that care is joined up
- Work with other professionals, agencies and organisations to maximise quality of life
- Act as a point of contact as things change
- Monitor how care is helping people to achieve the things that matter to them
- Share good practice to ensure that people’s needs are appropriately met across different settings.
4. Care in the last days of life
Social workers:
- Keep the focus on quality of life
- Ensure people have the information they need
- Deal with practical issues
- Provide emotional, social, cultural and spiritual support
- Ensure people are not alone if they don’t want to be.
5. Care after death
Social workers:
- Ensure people have the information and support they need to complete the associated formal processes and procedures
- Help people to find ways to live with loss
- Provide support for people who are left at risk as a result of losing someone
- Refer people for specialist support if they need this
- Provide emotional support to colleagues as part of developing a supportive reflective culture
- Share learning with others.
This is an extract from Association of Palliative Care Social Workers in collaboration with the former College of Social Work and Making Waves Lived Experience Network/OPEN FUTURES Research, with support from the British Association of Social Workers and Hospice UK (2016) The role of social work in palliative, end of life and bereavement care
Download the tool as a PDF
Tool 2: Learning needs analysis for social workers for end of life care
You can use this tool to consider how far you meet the capabilities for supporting people who are dying or bereaved, and to plan how you will gain skills, knowledge and confidence to work well in this area.
| Capability | How well I do this (1 low– 5 high) |
Comment | Action | By when | Complete? |
| Social workers are ready to apply their knowledge, skills and values to recognise and support people who are dying, facing loss or bereaved. | |||||
| Social workers recognise the impact of people’s values and beliefs, including their own, on death, dying and loss; and are committed to the principle of living well until you die, whatever that means for someone. | |||||
| Social workers value people as individuals, and ensure their wishes and needs are respected at end of life and when bereaved. | |||||
| Social workers ensure that people who are dying or bereaved, especially from marginalised or disadvantaged groups, can empower themselves and be enabled to get the support they need. | |||||
| Social workers are aware of the impact of loss from knowing that you are or someone close is dying, from physical and other changes, from grief and from bereavement. They know how to use law, evidence and systems to support and protect dying people and those close to them. | |||||
| Social workers are able to judge when specialist support is needed for people they work with who are dying or bereaved, and when they themselves need additional support. | |||||
| Social workers are able to engage with people who are dying or bereaved and those close to them to ensure they have the practical, emotional, psychological and spiritual support they need. This includes working with individuals, groups and communities. | |||||
| Social workers are able to access advice, information and input from palliative care social workers when this is needed in their organisation. | |||||
| Social workers remind others of the need to recognise and respond effectively to people who are dying and bereaved, act as mentors, and share learning about how to do this well. This includes advocating for people’s rights and supporting them to access the information and help they need. |
This is taken from Association of Palliative Care Social Workers in collaboration with the former College of Social Work and Making Waves Lived Experience Network/OPEN FUTURES Research, with support from the British Association of Social Workers and Hospice UK (2016) The role of social work in palliative, end of life and bereavement care http://www.apcsw.org.uk/resources/social-work-role-eol.pdf
Download the tool as a PDF
Tool 3: Starting the conversation
The National Council for Palliative Care (NCPC)
Someone you know is very ill.
They may not have long to live. You feel desperately sad, but also at a loss what to do. Their illness seems to have changed everything. How can you talk about things the way you used to? Will they still want to see you when time is so short? Should you call? And what can you possibly say to them under the circumstances?
![]() Download the leaflet Starting the conversation as a PDF file.
Download the leaflet Starting the conversation as a PDF file.
Download the tool as a PDF
Tool 4: Supporting older carers, spheres of support
This tool sets out ways of supporting older carers identified in pilots around the country. You can use it to consider how your service accesses or provides support for older carers, particularly when they are isolated and when they become bereaved.
Practical
Information and advice
Emotional
This tool is based on Age UK (2013) Supporting Older Carers of Those Nearing the End of Life, Lancaster University Evaluation of Six Pilot Projects. Final Report
Download the tool as a PDF
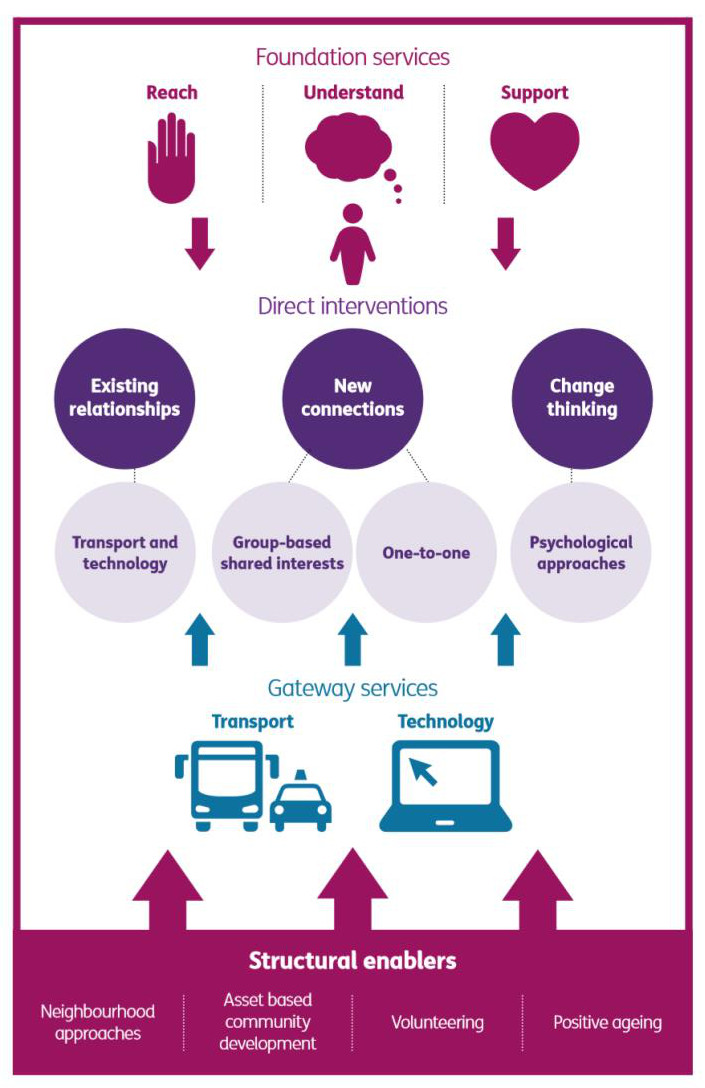
Reducing Loneliness
This tool presents a way of thinking about interventions to reduce loneliness along with some questions for reflection. You can use it to think about how your role and service works with older people to reduce loneliness.
How do you reach people, understand their situation and support them to take up services that help them to make meaningful connections?
How do you support people to maintain existing relationships, sustain new connections and change their thinking about their social connections?
How do you ensure access to transport and technology as a gateway to enabling social connections?
How do you use neighbourhood approaches, asset based community development, volunteering and positive ageing to empower people?
This is based on Age UK and The campaign to end loneliness (2015) Promising approaches to reducing loneliness in later life http://www.campaigntoendloneliness.org/loneliness-research/
Download the tool as a PDF
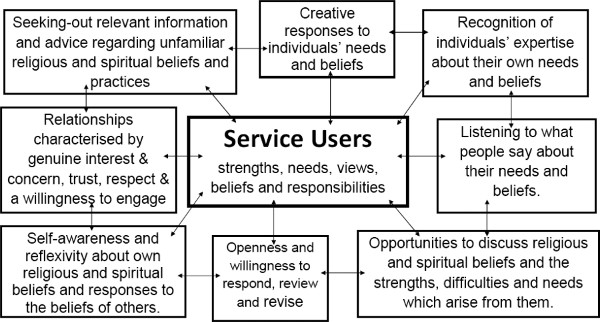
Tool 6: Principles for reflection on religion and belief
This tool sets out the principles that underpin good social work practice around religion and belief. You can use the questions below to reflect on your practice.
- Are you sufficiently self-aware and reflexive about your own religious and spiritual beliefs or the absence of them and your responses to others?
- Are you giving the individuals/ groups involved sufficient opportunities to discuss their religious and spiritual beliefs and the strengths, difficulties and needs which arise from them?
- Are you listening to what they say about their beliefs and the strengths and needs which arise from them?
- Do you recognise individuals’ expertise about their own beliefs and the strengths and needs which arise from them?
- Are you approaching this piece of practice with sufficient openness and willingness to review and revise your plans and assumptions?
- Are you building a relationship which is characterised by trust, respect and a willingness to facilitate?
- Are you being creative in your responses to individuals‟ beliefs and the strengths and needs which arise from them?
- Have you sought out relevant information and advice regarding any religious and spiritual beliefs and practices which were previously unfamiliar to you?
This tool is based on Furness S and Gilligan P (2010) Social Work, Religion and Belief: Developing a Framework for Practice, British Journal of Social Work, 40 (7), pp 2185-2202.
Text of the diagram (clockwise)
Clockwise:
- Seeking out relevant information and advice regarding unfamiliar religious and spiritual beliefs and practices
- Creative responses to individual’s needs and beliefs
- Recognition of individuals’ expertise about their own needs and beliefs
- Listening to what people say about their needs and beliefs
- Opportunities to discuss religious and spiritual beliefs and the strengths, difficulties and needs which arise from them
- Openness ad willingness to respond and revise
- Self-awareness and reflexivity about own religious and spiritual beliefs and responses to the beliefs of others
- Relationships characterised be genuine interest and concern, trust, respect and a willingness to engage
Centre:
Service Users
strengths, needs, views, beliefs and responsibilities