Download the whole case study as a PDF file
Eve is a carer for her father, who has early stage vascular dementia and numerous health problems. She has two children: a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15.
This case study considers issues around being a ‘sandwich carer’ – that is, caring for both a parent and a child – maintaining employment and working with a whole family including family group conferences, as well as the impact of dementia and the role of assistive technology.
When you have looked at the materials for the case study and considered these topics, you can use the critical reflection tool and the action planning tool to consider your own practice.
Name: Eve Davies
Gender: Female
Age: 42
Ethnicity: White British
Download resource as a PDF file
First language: English
Religion: None
Eve lives in a town. She has two children, a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15. Eve’s mother died four years ago, and her father, Geoff, lives close by. Geoff has early stage vascular dementia and numerous health problems relating to a heart attack he had two years ago. Eve works part time in an administration role at a local college. She has lost contact with her friends and lost touch with her hobbies (swimming and singing in a choir) because she has prioritised her family.
Matt is at college studying for his A levels. He is frustrated that his illness is interfering with all aspects of his life. Joanne is becoming more withdrawn and resentful as an increasing amount of Eve’s time is taken up with other family members. Geoff has started to neglect himself at home, and is finding it more difficult to carry out daily tasks. Following a social care assessment, he has a befriending service stop by every week and a homecare team each morning to check he’s ok and supervise his medication, which Eve sets up for them. The care agency have reported that there’s a possibility Geoff has been accessing his medication and taking it. Geoff remains adamant that he is fine, and with Eve’s support he can manage.
Eve is feeling stressed and isolated. She wants to increase her working hours for financial reasons, but is unable to as she needs to be available for Geoff. Eve is having problems with sleeping and feels generally run down, and recently has been suffering from stomach pain and nausea. She says that she feels ‘withdrawn from normal life.’ She tried attending a carers’ group but found that listening to other carers’ problems highlighted her own. Instead, she sometimes uses an online forum at night when everyone else is asleep.
Eve was recently referred by her GP for a carer’s assessment. You have been out to see her twice and talked to her children. You have completed the assessment and support plan with her.
Eve Davies
Download resource as a PDF file
What others like and admire about me
Good mum (mostly!)
I’m very organised
People can count on me
I help people out
I’m kind
I’m a good singer
What is important to me
My kids – I want them to be happy
Family time
Dad staying at home – I promised Mum
My job – people I work with
Health – exercise, sleep!
Just to know I’m not on my own
How best to support me
Listen to me and include me in your network
A bit of ‘me time’ to breathe – see friends, swimming, choir
Be honest about what you can do and do what you say you will
Don’t lumber your problems on me when there’s nothing I can do
Talk to me about me, not just about caring
Let me know who to contact
Don’t give me loads of information
Emails not phone please
Don’t arrange meetings when I’m at work
Help me plan so I can do everything!
Download resource as a PDF file
Name: Eve Davies
Gender: Female
Age: 42
Ethnicity: White British
First language: English
Religion: None
Date chronology completed 15 February 2016
Date shared with person 15 February 2016
| Date | Life Event | Outcome and/or response |
| 15.02.74 | Evelyn Mary Davies (known as Eve) born in Welsh border town. | |
| 12.04.96 | Married to Eric Sanderson and moved to Moreton. | |
| 26.07.98 | Birth of first child, son, Mathew Eric Sanderson. | |
| 18.09.00 | Birth of second child, daughter, Joanne Rachael Sanderson. | |
| 16.09.03 | Divorced. Reverted to maiden name though children retained their father’s name. | Eve and children remain in the marital home. Eve is proud of how well she has managed, with her part-time post which she enjoys and regular child support from the children’s father. Eve says she was not unduly concerned when initial fortnightly contact between the children and their father began to tail off. The children did not wish to travel to his new location some 50 miles away and he did not make sufficient effort in her view to see them. |
| 03.07.09 | Son, Matt, diagnosed with Crohn’s disease which causes him to frequently need the toilet, and have some faecal incontinence. He has relapses causing dramatic weight loss and frequent hospital admission. | Eve managed the health care and hospital appointments for her son as well as providing reassurance. Eventual diagnosis indicates a need for longer term health service involvement. Eve values the support of school nurse and feels that physically Matt’s illness is under control more now though the stigma and embarrassment of Matt’s illness has begun to take its toll on his emotional wellbeing. |
| 21.01.12 | Eve’s mother, Margaret, died suddenly in her sleep having suffered a heart attack. Eve herself is shocked by her mother’s death and describes her father as struggling to cope with his wife’s sudden death. | Eve now includes her father’s shopping in her weekly shop, prepares his evening meals, helps with laundry and other household chores, juggling this with her own chores and Matt’s health appointments. |
| 19.03.14 | Eve’s father, Geoff, had a heart attack. Hospitalised for two weeks whilst a stent was fitted and his recovery monitored. | His heart attack has left Eve’s father with numerous related health problems. Eve begins to manage of her father’s health appointments alongside management of Matt’s. Over the next year Geoff starts to have memory problems. |
| 16.11.15 | Eve’s father diagnosed with early stage vascular dementia.
Social care assessment undertaken. Befriending service and home care provision arranged.
|
Mixed service with Eve as main carer for her father, Geoff Davies, and some home care and befriending service provision to Geoff now in place. At this time Eve tried attending a carers’ group but found that listening to other carers’ problems highlighted her own. Instead, she sometimes uses an online forum at night when everyone else is asleep. |
| 29.01.16 | Eve attends her GP surgery as she is regularly feeling nauseous. The GP asked Eve if she is experiencing more stress than usual. Eve expresses concern that her father has started to neglect himself at home, and is finding it more difficult to carry out daily tasks. He gets confused with tasks like making a meal. Eve worries that he doesn’t eat properly. Sometimes he has trouble remembering words and this makes him feel cross. Eve explains that he sometimes now has short bursts of sudden confusion. She finds this frightening and her children do too, which worries her. | Following this discussion with Eve about the pressures on her at the moment and indications of stress causing her physical symptoms, with her agreement the GP has referred Eve for a social care assessment as carer for both her father and her son.
|
| 04.02.16 | Initial visit by social worker. SW sees Eve on her own at home. | SW makes another appointment to continue the assessment at a time when the children are at home to include them in the conversation. |
| 09.02.16 | Second visit to Eve and conversation with her children. | Carer’s assessment and support plan completed. SW arranges with Geoff that he will have an assessment in the next few weeks. |
| 15.02.16 | Paperwork completed. | Sent to Eve. |
Download resource as a PDF file
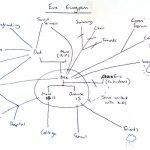
Eve’s Ecogram
Download resource as a PDF file
About me
Name Eve Davies
Address 1 Fir Avenue, Moreton, ZZ1 Z11
Telephone 012345 123456
Email eve.davies@parkcollege.ac.uk
Gender Female
Date of birth 15.2.1974 Age 42
Ethnicity White British
First language English
Religion None
GP Dr Tailor, Parkside Surgery
How would you like us to contact you?
Do you need any support with communication?
No
About the person/ people I care for
My relationship to this person Daughter
Name Geoff Davies
Address 1 Pine Avenue, Moreton, ZZ1 Z22
Telephone 012345 234567
Gender Male
Date of birth 8.1.1943 Age 73
Ethnicity White British
First language English
Religion Baptised C of E
GP Dr Tailor, Parkside Surgery
Please tell us about any existing support the person you care for already has in place. This could be home care, visits or support from a community, district or community psychiatric nurse, attending any community groups or day centres, attending any training or adult learning courses, or support from friends and neighbours.
Home care every morning for medication and check up
Befriending service 2 hours a week
GP
My relationship to this person Mother
Name Matt Sanderson
Address 1 Fir Avenue, Moreton, ZZ1 Z22
Telephone 012345 234567
Gender Male
Date of birth 26.7.1998 Age 17
Ethnicity White British
First language English
Religion None
GP Dr Tailor, Parkside Surgery
Please tell us about any existing support the person you care for already has in place. This could be home care, visits or support from a community, district or community psychiatric nurse, attending any community groups or day centres, attending any training or adult learning courses, or support from friends and neighbours.
Goes to college (doing A levels)
GP and nurse at the surgery
Consultant at the hospital
The things I do as a carer to give support
Please use the space below to tell us about the things you do as a carer (including the emotional and practical support you provide such as personal care, preparing meals, supporting the person you care for to stay safe, motivating and re-assuring them, dealing with their medication and / or their finances).
Dad has early stage vascular dementia and numerous health problems relating to a heart attack he had two years ago. He has started to neglect himself at home, and is finding it more and more difficult to carry out daily tasks. He gets confused with cooking or tasks like making a meal. Sometimes Dad has trouble remembering words and this makes him feel cross. On occasion he does experience short bursts of sudden confusion, which can be frightening for other family members.
Following a social care assessment, he has a befriending service stop by every week and a homecare team each morning to check he’s ok and supervise his medication.
This is what I do for Dad:
- Preparing Dad’s medication for the day – setting out in reminder containers
- Greeting care workers in the morning
- Remind Dad about having a wash
- Leave lunch in fridge
- Remind Dad about appointments
- Visit in the evening and cook dinner
- Sort out problems with the care agency
- Do shopping, cleaning, laundry
- Collect medication
- Check for medical appointments/ reviews
- Take Dad to appointments
- Sort out Dad’s mail – pay bills
- Fix things round the house
- Sort out extra care if Matt is in hospital
Matt has Crohn’s disease. He is at college studying for his A levels. He is doing well but his illness does interfere with his life and he can get frustrated about this. He wants good grades to be able to become a journalist and move abroad. It is embarrassing for him that he has to frequently rush to the toilet, and occasionally he is incontinent. Matt has regular relapses. This causes him to lose a lot of weight and he has been in hospital three times in the last year and missed college.
This is what I do for Matt:
- In the morning, make special lunch and ensure that he has his emergency bag (extra clothing, wipes, plastic bag and air freshener)
- Remind him about his weekly blood test appointment.
- Extra washing
- Help with homework
- Transporting Matt to hospital/GP/nurse appointments.
I also look after my daughter Joanne who is 15.
How my caring role impacts on my life
Please use the space below to tell us about the impact your caring role has on your life.
Like all working mums I have a lot on. As I have had to do more for Dad, it has got more difficult to juggle family chores and work.
I want to increase my working hours for financial reasons but I don’t see how I can at the moment, as Dad’s care needs are increasing and I need to be available for him. I’ve had to take some flexible working hours recently to cover last minute changes in arrangements for Dad’s care. I frequently have to take phone calls at work about care arrangements. I am concerned that I won’t be able to keep working and we need the money.
I’m worried that Dad isn’t eating properly. The care agency have reported that the medication audit has shown that Dad might have been taking his medication at the wrong times. Dad doesn’t want to talk about longer term planning and making advanced decisions. He does not want any more social care provision in the house. This really worries me particularly as Dad will need more help as time goes on. Also if Dad suddenly needed a lot more help or I was unwell then I am not sure how we would manage.
I want Matt to be able to manage his illness better so that he is happier and able to do the things he wants. As I have had to spend more time with Dad and Matt, my daughter Joanne has become more distant. She finds it difficult that we need to work around what Matt needs, for example for meals. Joanne has always been helpful but has become more withdrawn and resentful. She has started to hang around with older teenagers, and I’m worried they might be ‘leading her astray’. She has had a few letters from school mentioning poor attendance and a drop in her grades. I feel like I don’t have time at the moment to be a good mum.
I’m having problems with sleeping and feel generally run down, and recently I have had to see the GP about stomach pain and nausea, which she thinks is to do with stress. I feel like I don’t have any time now to just breathe and am withdrawing from normal life. I don’t currently have time to exercise – I used to swim, or to sing in the choir. I’ve also lost contact with friends so I feel quite isolated.
What supports me as a carer?
Please use the space below to tell us about what helps you in your caring role.
I sometimes go on an online carers’ forum at night when everyone else is asleep and that’s quite helpful. I did try attending a carers’ group but it got me down listening to other people’s problems.
Work gives me a bit of a break from caring and my boss has so far been quite supportive with flexible working though I don’t want to push it.
Matt’s nurse at the GP surgery has been really helpful with information and support. Matt gets on with her well.
My feelings and choices about caring
Please use the space below to tell us about how you are feeling and if you would like to change anything about your caring role and your life.
It’s my choice to care for my family and I want to keep on doing that, and be a good mum and a good daughter.
If I knew that Dad was getting the care he needs and that we had a plan for the future then I would manage much better.
At the moment I’m feeling stressed and quite overwhelmed. There’s always something else to sort out. I feel like I don’t have anyone to support me. I miss my Mum and worry about whether I’m looking after my Dad as well as she did.
I want to know my family is ok. I don’t want to stop looking after my kids and my Dad.
I want to be able to manage my different roles at home and at work, and to do things well.
I want to have more time with my children and we want more time as a family.
I would love to increase my hours at work.
I’d like to start swimming and join the choir again. I’d like to see friends sometimes.
I do need more sleep.
Information, advice and support
Let us know what advice or information you feel would help you and what sort of support you think would be beneficial to you in your caring role.
Someone to talk to Dad about getting the care he needs – particularly to ensure he takes the right medication and that he eats enough.
Some help with planning Dad’s care in case there is a crisis, and to plan ahead for what he will need in the future.
Someone to check on Dad when I’m at work.
A break – just to be free without interruptions.
Some back-up so that I am not always on call.
Someone to talk to about how to manage all of this.
Someone for Joanne to talk to if she wants to.
Someone to support Matt to manage his illness so he can achieve his aims.
Conclusion
To be used by social care assessors to consider and record measures which can be taken to assist the carer with their caring role to reduce the significant impact of any needs. This should include networks of support, community services and the persons own strengths. To be eligible the carer must have significant difficulty achieving 1 or more outcomes without support; it is the assessors’ professional judgement that unless this need is met there will be a significant impact on the carer’s wellbeing. Social care funding will only be made available to meet eligible outcomes that cannot be met in any other way, i.e. social care funding is only available to meet unmet eligible needs
Date assessment completed 15 February 2016
Social care assessor conclusion
Eve is providing significant support to her father and her two children, one of whom has Crohn’s disease. Eve also works part-time. Eve’s father has some support from home care and a befriending service. Her son has support from health services. Eve is very organised, and juggles chores and work well. However, she says that she is starting to feel increasingly stressed and this is having an impact on her health. She is also quite isolated and has no time at present to have a break from caring. Eve would like to continue supporting her family and increase her working hours, as well as having some time for her own interests. It is important to Eve that her father remains at home and is safe, and that her children are happy. Eve would benefit from support to enable her to manage the demands on her, and to have some time for herself. She would also benefit from some emotional support for her and for her family. This will enable her to continue as a carer and to improve her health and wellbeing.
Eligibility decision Eligible for support
What’s happening next Create support plan
Carry out assessment for Mr Geoff Davies
Completed by
Name
Role
Organisation
Signing this form (for carer)
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Name
Signature
Download resource as a PDF file
About me
Name Eve Davies
Address 1 Fir Avenue, Moreton, ZZ1 Z11
Telephone 012345 123456
Email eve.davies@parkcollege.ac.uk
Gender Female
Date of birth 15.2.1974 Age 42
Ethnicity White British
First language English
Religion None
GP Dr Tailor, Parkside Surgery
About the person/ people I care for
My relationship to this person Daughter
Name Geoff Davies
Address 1 Pine Avenue, Moreton, ZZ1 Z22
Telephone 012345 234567
Gender Male
Date of birth 8.1.1943 Age 73
Ethnicity White British
First language English
Religion Baptised C of E
GP Dr Tailor, Parkside Surgery
My relationship to this person Mother
Name Matt Sanderson
Address 1 Fir Avenue, Moreton, ZZ1 Z22
Telephone 012345 234567
Gender Male
Date of birth 26.7.1998 Age 17
Ethnicity White British
First language English
Religion None
GP Dr Tailor, Parkside Surgery
Support plan completed by
Name
Role
Organisation
Support Plan
| Needs | Outcomes | Actions
|
| To know that her Dad has the support that he needs | Mr Davies takes correct medication
Mr Davies eats enough to stay well Mr Davies has support to manage meals and personal care |
To talk to Mr Davies about increasing his support around meals
To talk to Mr Davies about installing assistive technology – reminder for meals and tasks |
| To know that Dad has plans in place for future needs | Everyone to know what to do if there is a crisis
To have a plan for future care for Mr Davies |
Hold a family group conference to talk about contingency plans and plans for the future |
| To be able to do her job well and enjoy it | Increase her work hours
Not be interrupted at work as much |
Care workers to manage the service without calling on Eve by reporting to one supervisor who will deal with questions or concerns
|
| To have more time with her children and for herself | Have dinner with the kids three nights a week
See friends once a month Go to choir once a fortnight |
Direct payment for neighbour to do cleaning and laundry for Eve
Talk to Mr Davies about building links with former colleagues and community groups with a view to future breaks for Eve |
| To have someone to talk to about caring | Feel more supported | Keep using the online forum
Provide information about the carers’ helpline |
| To be able to support Joanne properly | Joanne attending school and doing well | Eve to talk to school about family situation
Arrange for Joanne to talk to young carer’s group if she wants to |
| To be able to advise Matt about how to manage his illness | Matt not going to hospital as often | Contact the practice nurse to talk to Matt about expert patient programme and Chron’s support group |
| To stay healthy | Having enough sleep
Not waking up stressed |
GP is now aware that Eve is a carer and this is flagged on her notes
Go swimming once a week |
Date of support plan: 15 February 2016
This plan will be reviewed on: 15 February 2017
Signing this form
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Name
Signature
Eve has given consent to share this support plan with Mr Davies. This support plan will link into his assessment.
Sandwich caring
The Care Act places a duty on local authorities to assess adult carers, including parent carers of disabled and other children in need, before the child they care for turns 18, so that they have the information they need to plan for their future. Guidance, advocating a whole family approach, is available to social workers (LGA 2015, SCIE 2015, ADASS/ADCS 2011).
- Carers UK (2012) Sandwich caring
- Circle (2018) Supporting carers to work and care
- Think Local Act Personal (2017) Supporting working carers
- Mumsnet for the Care Quality Commission August (2014) Care Quality Commission: Sandwich Generation Survey Summary Report
- Institute for Public Policy Research (2013) The sandwich generation: older women balancing work and care
- Carers UK (2014) Carers at breaking point
- Blog: Impact of cuts
Carers’ employment
Research shows that both emotional and practical support from social workers are valuable, for example when looking at what was valued by the mothers of transition-age children with mental illness (Gerten and Hensley 2014) and by men as caregivers to the elderly (Collins 2014).
- Skills for Care (2013) Balancing work and care
- Carers UK (2015) Caring and isolation in the workplace
- Carers UK (2014) The case for care leave
- Carers UK (2014) Supporting employees who are caring for someone with dementia
- Carers UK (2013) Supporting working carers
- NIHR (2014) Improving employment opportunities for carers: identifying and sharing good practice
- Department of Health (2015) Pilots to understand how to support carers to stay in paid employment
Tool
- Tool 1: Support for carers in employment
Life course and whole family approaches
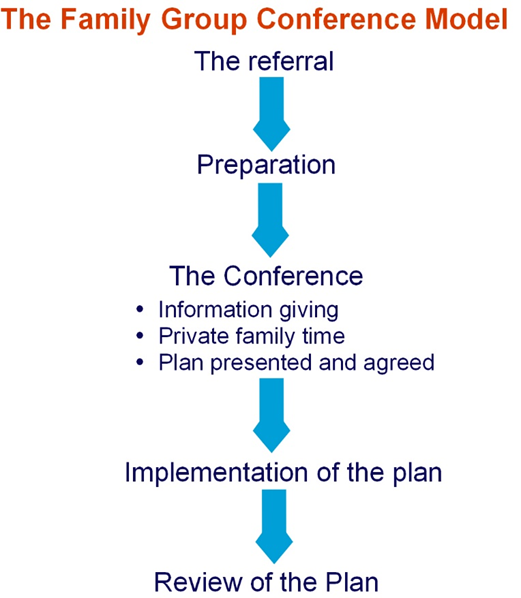
The whole family approach is a strong theme in the research (LGA 2015) along with relationship based practice (SCIE 2016, Cooper 2015, Wilson et al 2011, Ruch et al 2010). Family group conferencing, along with mediation as whole family approaches, were found to have particular applicability to adult safeguarding social work. (SCIE 2012).
- Beth Johnson Foundation (2014) A life course approach to promoting positive ageing
- SCIE (2012) At a glance 62: Safeguarding adults: Mediation and family group conferences
- Hobbs A and Alonzi A (2013) Mediation and family group conferences in adult safeguarding, Journal of Adult Protection, 15(2), pp.69-84
- Carers Trust Whole family approach – practice examples
Tool
- Tool 2: Family group conferences
Assistive technology
Evidence points to the need for social work teams are to have good information about the support available to carers. National materials offer a valuable resource to social workers seeking to research how to work with their clients and their carers which can be supplemented locally and from the active contributions of the ‘online’ community (Young Sam Oh 2015).
- SCIE (2010) At a glance 24: Ethical issues in the use of telecare
- Carers UK and Tunstall (2013) Potential for Change: Transforming public awareness and demand for health and care technology
- Carers UK and Tunstall (2012) Carers and telecare
- Carers UK (2012) Future care: Care and technology in the 21st century
Video
- SCIE (2010) Telecare videos
Tool
- Tool 3: Ethics of assistive technology
Dementia
Research suggests an assets or strengths based approach to social work support with the person and their family and/or network of support. The Manual for good social work practice (DH 2015) uses a timeline as a model that can underpin how the social worker supports and intervenes, from early preventative measures through various stages of loss towards end-of-life. Three critical points on the timeline – diagnosis, taking up active caring and the decline of the person’s capacity – are identified. It is important for social workers to assess the carers needs, sustain the carers own identity, develop and maintain their network of support and resources, and access financial and legal advice.
- SCIE Dementia GatewayDepartment of Health (2015) TCSW (2015) A manual for good social work practice: Supporting adults who have dementia, The College of Social Work
- Carers Trust (2014) The Triangle of Care: Carers Included: A Guide to Best Practice for Dementia Care
- Carers Trust (2013) A Road Less Rocky – Supporting Carers of People with Dementia
- Alzheimer’s Research UK (2015) Dementia in the family: the impact on carers
Tool
- Tool 4: Triangle of care – self-assessment for dementia professionals
Carers Trust (2014) The Triangle of Care: Carers Included: A Guide to Best Practice for Dementia Care (Page 22 Self-assessment tool for organisations)
Download resource as a PDF file
Tool 1: Support for Carers in Employment
You can use this tool with carers to think about what would support someone to manage work and caring responsibilities.
| What helps?
|
What is this like for me? | What can I do about it? |
| Supportive manager
|
||
| Flexible/ special leave arrangements
|
||
| Flexible working hours
|
||
| Remote working
|
||
| Information and support for carers at work
|
||
| High quality, appropriate care and support
|
||
| Support from relatives and friends
|
||
| Services that are available outside working hours
|
||
| Help with coordinating care and support
|
||
| Advice and information about legal & money issues
|
This tool is based on research about what helps carers who are working (Carers UK (2015) Caring and isolation in the workplace).
Download resource as a PDF file
Tool 2: Family Group Conference
This tool sets out the process for a Family Group Conference. You can use it to plan and hold a conference.
The Family Group Conference process
Stage 1: The referral
Whether or not a family group conference takes place is a decision made by the family. Under no circumstances can a family be made or forced to have a family group conference.
Once a referral for a family group conference is made, there will need to be a co-ordinator to liaise with the family.
The co-ordinator helps the family to plan the meeting and chair the meeting. The co-ordinator is different from the referrer and acts as a neutral person. The co-ordinator will not influence the family to make a particular decision but will help them to think about the decisions that need to be made. Families should be offered the opportunity to request a co-ordinator who suitably reflects their ethnicity, language, religion or gender, and the family’s request should be accommodated wherever possible.
Stage 2: Preparation
The co-ordinator organises the meeting in conjunction with the family members and other members of the network. This can include close friends.
- The co-ordinator discusses with the person with care and support needs how they can be helped to participate in the conference and whether they would like a supporter or advocate at the meeting . The supporter/advocate will then meet with them in preparation for the meeting.
- The co-ordinator meets with members of the family network, discusses worries or concerns, including how the family group conference will be conducted, and encourages them to attend.
- The co-ordinator liaises with the referrer and other relevant agencies to ensure family members have appropriate information about:
- the wellbeing concerns which need to be considered at the family group conference. This includes identifying any bottom line about what can, and, importantly, cannot be agreed as part of the plan from the agency’s perspective.
- services that could help.
- The co-ordinator negotiates the date, time and venue for the conference, sends out invitations and makes the necessary practical arrangements.
Stage 3: The conference
The family group conference follows three distinct stages.
a) Information giving
This part of the meeting is chaired by the co-ordinator. They will make sure that everyone is introduced, that everyone present understands the purpose and process of the family group conference and agrees how the meeting will be conducted including, if felt helpful by those present, explicit ground rules. The service providers give information to the family about:
- the reason for the conference;
- information they hold that will assist the family to make the plan;
- information about resources and support they are able to provide;
- any wellbeing concerns that will affect what can be agreed in the plan; and
- what action will be taken if the family cannot make a plan or the plan is not agreed.
The family members may also provide information, ask for clarification or raise questions.
b) Private family time
Agency staff and the co-ordinator are not present during this part of the conference. Family members have time to talk among themselves and come up with a plan that addresses concerns raised. They will identify resources and support which are required from agencies, as well as within the family, to make the plan work.
c) Plan and agreement
When the family has made their plan, the referrer and the co-ordinator meet with the family to discuss and agree the plan including resources.
It is the referrer’s responsibility to agree the plan of action and it is important that this happens on the day of the conference. It should be presumed that the plan must be agreed unless it puts anyone at risk of significant harm. Any reasons for not accepting the plan must be made clear immediately and the family should be given the opportunity to respond to the concerns and change or add to the plan.
It is important to ensure that everyone involved has a clear understanding of what is decided and that their views are understood.
Resources are discussed and agreed with the agency concerned, and it is important that, at this point, timescales and names of those responsible for any tasks are clarified. Contingency plans, monitoring arrangements and how to review the plan also need to be agreed.
The co-ordinator should distribute the plan to family members involved and to the social worker and other information givers/relevant professionals.
1.3.5 Stage Three: Implementation of the Plan
It is essential that everybody involved implements their parts of the plan within agreed timescales and communicate and addresses any problems that arise.
1.3.6 Stage Four: Review of the plan
There should be a clear process for reviewing the implementation of the plan. A review family group conference or other meeting should be offered to the family so they can consider how the plan is working, and to make adjustments or change the plan if necessary.
This information is based largely on the Family Rights Group’s Family Group Conference Process
Download resource as a PDF file
Tool 3: Ethics of using assistive technology
This tool highlights the ethical issues of using assistive technology. You can use it to consider when assistive technology would be beneficial for someone, and to reflect on the benefits and drawbacks of it more generally.
What are the ethical issues about using assistive technology (AT) to support carers?
This tool is based on SCIE At a glance 24: Ethical issues in the use of telecare

Download The Triangle of Care as a PDF file
The Triangle of Care
Carers Included: A Guide to Best Practice
in Mental Health Care in England
The Triangle of Care is a therapeutic alliance between service user, staff member and carer that promotes safety, supports recovery and sustains wellbeing…